Global Mortality
Respiratory health issues, including diseases caused by respiratory
viruses, exposure to smoke, dust, and other airborne pollutants,
contribute significantly to global mortality. Here's a summary of the
estimated annual deaths associated with these factors:
| Cause | Estimated Annual Deaths | Notes |
| Air Pollution (Outdoor and Indoor Combined) | ~7 million | Includes deaths from heart disease, stroke, COPD, lung
cancer, and acute respiratory infections. |
| Chronic Respiratory Diseases (CRDs) | ~4 million | Includes conditions like chronic obstructive pulmonary
disease (COPD) and asthma. |
| Lower Respiratory Infections | >4 million | Primarily pneumonia and other acute infections. |
| Tuberculosis (TB) | ~1.4 million | One of the most common lethal infectious diseases. |
| Lung Cancer | ~1.8 million | Leading cause of cancer-related deaths. |
| Household Air Pollution | ~3.2 million | Resulting from cooking with polluting fuels and technologies. |
Notes:
- Overlap in Categories: It's important to note that these
categories are not mutually exclusive. For instance, air pollution is
a significant risk factor for both chronic respiratory diseases and lung
cancer. Therefore, simply summing these figures would lead to double-counting.
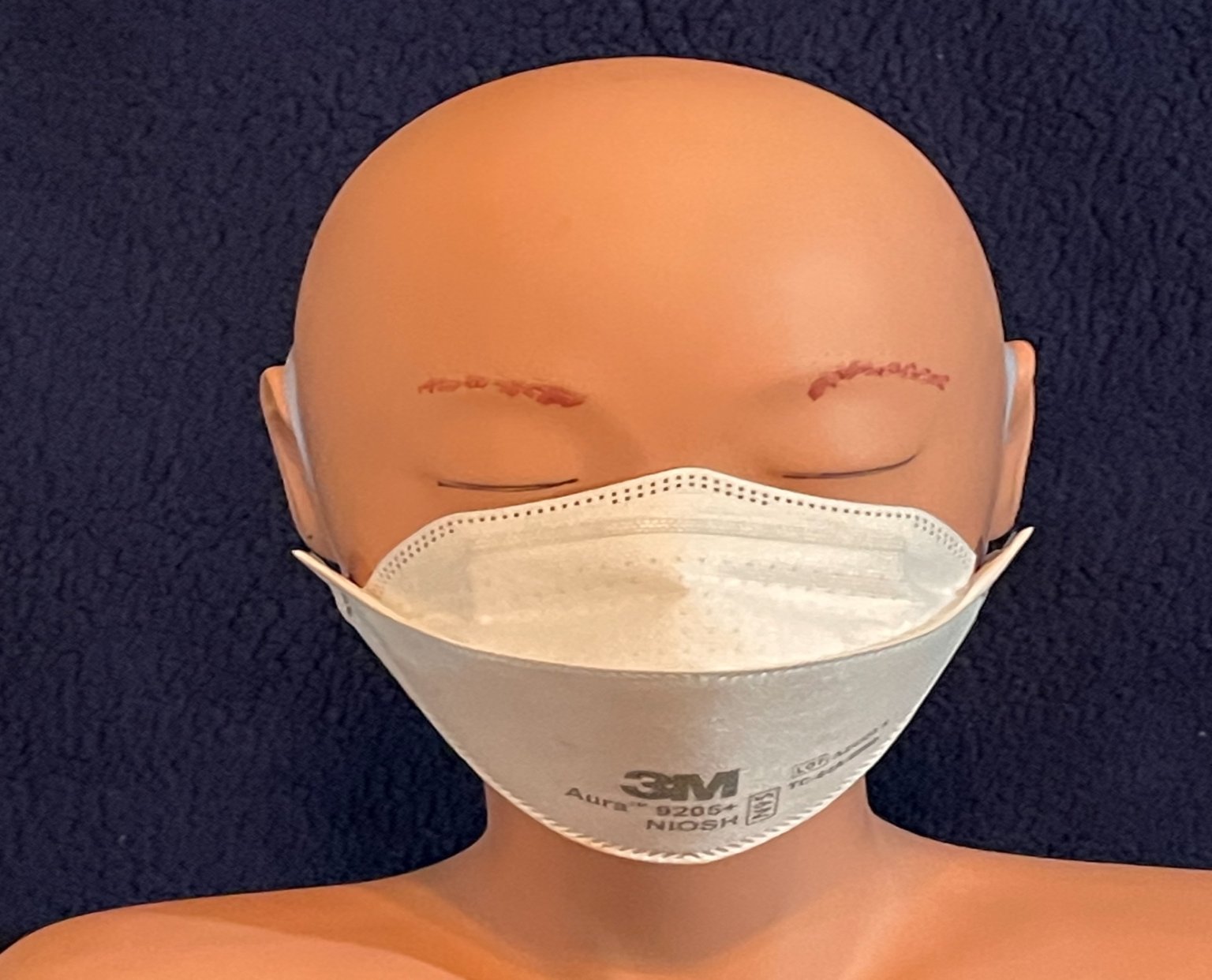
- Use of Masks: Masks are commonly used to protect against
airborne particles, including those from smoke, dust, and pathogens responsible
for respiratory infections. While they can reduce exposure and potentially
lower the risk of developing related health issues, their effectiveness
varies based on the type of mask, proper usage, and the specific pollutant
or pathogen.
Addressing these respiratory health challenges requires a multifaceted
approach, including reducing air pollution, improving indoor air
quality, promoting vaccination against respiratory pathogens, and
encouraging the use of appropriate respiratory protection when
necessary.
Example
Because we can't see all the stuff in the air around us, most of us
have a false sense of security when we are in a room with other
people for a long time. Our bodies are wonderfully capable of
handling small doses of viruses and other exposures, but we can't
handle new viruses and virus mutations, resulting in the occasional
pandemic. And some of us have weaker immune systems and can't handle
the exposures as well.
The following discusses Covid-19, the novel (new) coronavirus that
swept the world in 2020. The American Lung Association says,
"Rhinovirus is the most common cause, accounting for 10 to 40
percent of colds. Other common cold viruses include coronavirus and
respiratory syncytial virus (RSV)." And of course, influenza is a
virus.
Virus Concentration
One study reported the number live copies of the Covid-19 virus in
the oral fluid to be at least 7 million per milliliter (35 million
per teaspoon). Respiratory viruses are created in the breeding
ground of ideal temperature and moisture conditions in the sinus
cavities behind our noses.
When we breathe, we expel water droplets. The biggest droplets are
likely to fall to the ground within 1 to 2 meters, where they
quickly die. But the smallest droplets (especially from a cough) go
out as very tiny droplets, called a fog or mist or aerosol. The
aerosol can hang in a room for hours and hours. One study measured
0.87 copies of the live virus per liter in a room containing someone
infected with Covid-19. That may not seem huge, but 200 square foot
room with an 8 foot ceiling contains 45,000 liters of air and would
thus contain about 40,000 copies of the live virus.
Breathing Rate and Exposure
The breathing rate for adults is in the range of 12 to 18 breaths
per minute. The following example assumes 15. Each time we inhale,
we suck in about half a liter of air. That means we inhale 450
liters (120 gallons) of air per hour, containing about 400 live
viruses. Each person in the room is respirating (breathing) 1% of
the entire room volume. If there are 10 people in the room, together
they breathe 10% of the air in the room every hour, or 100% after
the room has been occupied for 10 hours. Without MyAirHat™, every
person in the room is continually inhaling the air into which the
other nine people are exhaling.
One study found that hospital restroom and break areas were the most
likely places for hospital workers to catch Covid-19. If you only
wear a MyAirHat when you go into a public restroom, you might
significantly reduce your risk of contracting a virus.
Example Summary
In this example, based on the extensive real-world testing discussed
earlier, you would inhale 228 viruses (57% of 400) if you wore an
N95 mask or only 76 viruses (19% of 400) if you wore a MyAirHat.
After 10 hours the difference is 2,280 compared to 760. The higher
virus load significantly increases the risk of serious illness or
death.
The same example would apply to smoke or other particles. If you are
trying to escape a burning skyscraper, the difference could mean
succumbing to smoke inhalation or survival.